John Paul Gallardo, D.D.S., P.A., Periodontics and Implant Dentistry
From Our Office
to Yours….
In 2007, the American Heart Association (AHA) published guidelines that significantly scaled back the underlying conditions for which antibiotic prophylaxis prior to certain dental procedures was recommended, leaving only four categories thought to confer the highest risk of adverse outcome:
In May, 2021, the AHA reviewed and upheld the 2007 guidelines, finding no convincing evidence that the frequency, morbidity, or mortality of infective endocarditis has increased since 2007.
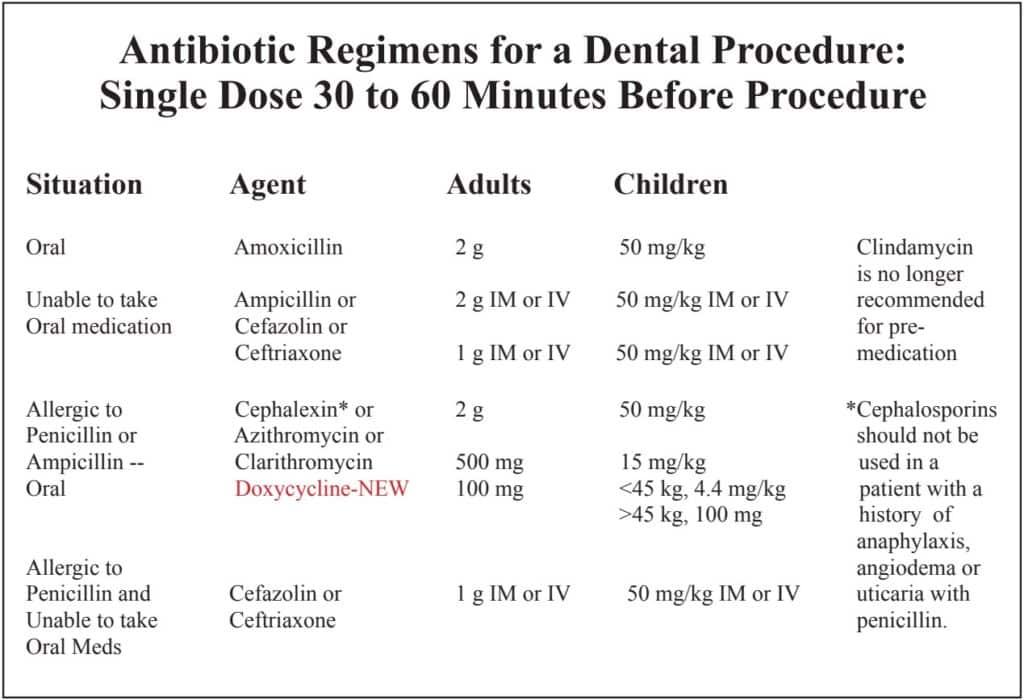
In addition, the AHA and two other professional organizations also published new research and guidelines for the use and contraindications of specific antibiotics prior to and following dental treatment.
Practitioners may be unaware of this new information and research. This issue of The PerioDontaLetter presents these latest findings and recommendations. For any questions about these recommendations, please contact our office.
Antibiotic Recommendations Prior to and Following Dental Treatment Have Changed
Recommendations for the antibiotic prophylaxis prior to certain dental procedures have existed historically for two groups of patients:
- Those with heart conditions that may predispose them to infective endocarditis, and
- Those with a prosthetic joint(s) who may be at risk for developing hematogenous infections at the site of the prosthetic device. The 2021 updated American Heart Association (AHA) and American Dental Association
(ADA) guidelines only recommend prophylaxis for patients with:
- Prosthetic cardiac valves, including transcatheter-implanted prostheses and homografts
- Prosthetic material used for cardiac valve repair, such as annuloplasty rings and chords
- A previous history of infective endocarditis
- A cardiac transplant with valve regurgitation due to a structurally abnormal valve
- The following congenital (present from birth) heart diseases: unrepaired cyanotic congenital heart disease, including palliative shunts and conduits, and any repaired congenital heart defect with residual
shunts or valvular regurgitation at the site of, or adjacent to the site of, a prosthetic patch or a prosthetic device. In upholding these guidelines in 2021, the AHA, along with the American Academy of Orthopedic Surgeons (AAOS) and the ADA also made the following recommendations for and against the use of specific antibiotics.
- The AAOS no longer recommends premedicating patients with joint replacements, except for those with a previous joint infection, or if the time since surgery is less than one year and the surgeon specifically recommends it.
- The AHA and AAOS and the ADA recommend using azithromycin, doxycycline, or cephalexin (if no history of anaphylaxis or angioedema) as alternatives for penicillin-allergic patients.
- C e p h a l e x i n ( K e f l e x ) i s recommended for patients with possible penicillin allergy, unless there is a previous history of anaphylaxis or angioedema.
- Serious, sometimes fatal, adverse reactions to clindamycin related to Clostridium difficile (C. difficile) have been reported. Consequently clindamycin is not recommended for antibiotic prophylaxis for dental procedures.
- Azithromycin has been associated with cardiovascular mortality. It should be avoided in patients with cardiovascular disease, especially arrythmias.
- The U.S. Food and Drug Administration (FDA) has updated fluoroquinolone labels to emphasize the risks of disabling adverse events. They should rarely be used, and then only when there are no alternative options for specific dental infections, sinusitis, bronchitis, and urinary tract infections.
Preventing Infection Of Prosthetic Joints And Other Types of Orthopedic Hardware
Based on research by Berberi et al through August of 2021, the American Academy of Oral Medicine, (AAOM), the ADA in conjunction with the AAOS, and the British Society for Antimicrobial Chemotherapy all advise against the universal use of antimicrobial prophylaxis prior to dental procedures for the prevention of prosthetic joint infections.
Overdiagnosis of Penicillin Allergy
Leads to Costly, Inappropriate Treatment
It has been reported that the overdiagnosis and misdiagnosis of penicillin allergy can lead to inappropriate and costly treatment. In November 2018, the Journal of the American Medical Association (JAMA) reported:
- As few as ten percent of all patients reporting penicillin allergy are truly allergic to penicillin.
- Only three cases of anaphylaxis to cephalosporins was reported for a group of 65,000 patients who reported allergy to penicillin. This is no greater than that reported by patients not allergic to penicillin.
- There is a less than five percent chance of patients allergic to penicillin reporting an allergic reaction when taking Keflex.
- The use of clindamycin was associated with a fourfold increase in surgical site infection compared with
the use of beta-lactam antibiotics (penicillin, Keflex, etc.). This is yet further evidence to support NOT choosing clindamycin for prophylaxis, or to prevent or treat infections.
Risk of Adverse Reactions to Oral Antibiotics Prescribed by Dentists
Thornhill reported 2.9 million serious negative reactions and 12,800 deaths in the US due to the use of clindamycin. In patients with no history of penicillin allergy or those taking methotrexate, amoxicillin has a very high reported level of safety.
Eliminate Quinolones As a Choice of Antibiotic
There are four FDA Black Box Warnings associated with the use of ciprofloxacin, levofloxacin and moxifloxacin including the following: tendon ruptures/tendinitis, peripheral neuropathy, and central nervous system disorders — confusion, tingling and psychosis, exacerbation of myasthenia gravis, and aortic aneurysm/dissection.
Conclusion
For all of the reasons enumerated above, one should employ a significantly heightened awareness regarding the possible negative sequelae of prescribing antibiotics. With a clear understanding of the many potential problems associated with prescribing ANY antibiotic and the new data which has been reported, the informed clinician can assist their patients with well-considered decisions regarding their use.

John Paul Gallardo, D.D.S., P.A., Periodontics and Implant Dentistry
Compliments of Dr. John Paul Gallardo
New AHA-ADA Pre-Medication Recommendations
Updated November, 2021
Journal of the American Dental Association
The 2021 updated American Heart Association (AHA) and American Dental Association (ADA) guidelines recommend antibiotic prophylaxis only for patients with:
- Prosthetic cardiac valves, including transcatheter-implanted prostheses and homografts.
- Prosthetic material used for cardiac valve repair, such as annuloplasty rings and chords.
- A history of infective endocarditis.
- A cardiac transplant with valve regurgitation due to a structurally abnormal valve.
- The following congenital (present from birth) heart disease:
- Unrepaired cyanotic congenital heart disease, including palliative shunts and conduits.
- Any repaired congenital heart defect with residual shunts or valvular regurgitation at the site of or adjacent to the site of a prosthetic patch or a prosthetic device.