From Our Office to Yours…
As dentists specializing in the treatment of diseases of the oral cavity and its associated structures, we are often also called upon to treat painful oral lesions in the mouth. This issue of The PerioDontaLetter contains guidelines on how to treat these common oral lesions.
The back page of this issue contains a table summarizing the confusing array of bisphosphonates and monoclonal antibodies which are used to treat osteoporosis and bone cancer. This table includes the route these drugs are administered and their likelihood of causing drug-induced osteonecrosis of the jaws — a side effect that we clinicians need to be aware of in treating our patients who are taking these drugs.
We hope you find this information helpful.
As always, we welcome your comments and questions.
Patients frequently present with painful oral lesions. These are usually not serious, but they appreciate our attention to them, our reassurance that they are not serious, and specific prescriptions for treatment. There is usually no cure, but there are treatments that shorten their duration and reduce the pain. Some of these are recurrent and others are self-induced traumatic lesions such as toothbrush trauma and burns from hot foods. Always be mindful of looking for oral cancer, and biopsy any suspicious lesions.
Treating Cold Sores And Canker Sores
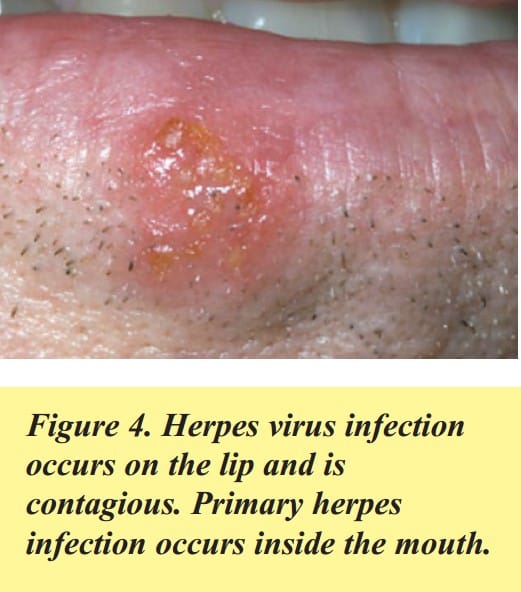
If the sore is on the lip, it is caused by a herpes simplex virus infection and is contagious. These are commonly called “cold sores” or “fever blisters.” Patients should avoid touching them and then touching their eyes since the herpes virus can spread to adjacent skin and to the eye and then is much more difficult to treat.
Treatment: Over-the-counter Abreva cream applied five times a day will shorten their duration. Over-the-counter Carmex lip balm applied at the first tingle will help the pain. Valtrex can be prescribed — two grams in the morning and two grams in the evening — taken at the first sign of an outbreak. Zovirax or Denavir ointments can also be prescribed, but are very expensive ($800-$900 per tube) and often not covered by medical insurance. A local compounding pharmacist can make up a much less expensive generic version of Zovirax (5.5% acyclovir ointment).
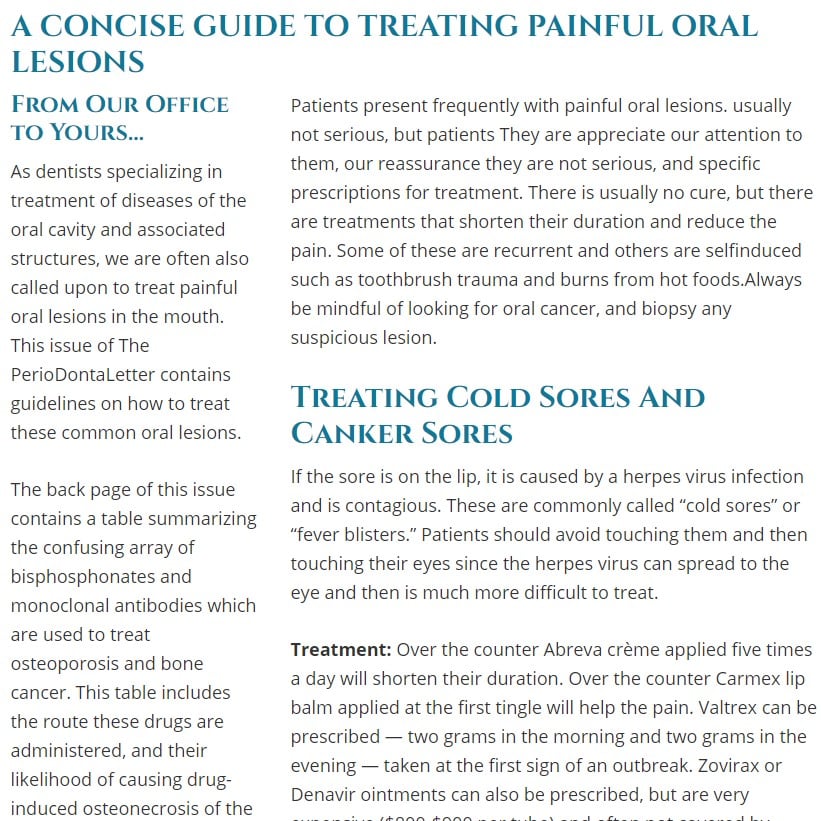
The most common sore inside the mouth is an aphthous ulcer, commonly called a canker sore. These are not viral. They occur on movable tissue like the tongue or cheeks and are not contagious. The cause is unknown and they tend to recur.
Treatment for a single lesion includes the application of over-the-counter (OTC) Zilactin B, Canker-X, Orajel with benzocaine, or prescription Orabase with the steroid Kenalog. These topical treatments coat and numb the lesion. The prescription steroid ointment Lidex is another treatment option. In the office, Debacterol can be applied which will cauterize the lesion and reduce the pain.
For multiple canker sores, treatment with a mouth rinse such as the “Magic Mouthwash” containing Benadryl, Maalox, and viscous xylocaine will reduce pain dramatically. For larger outbreaks, the steroid dexamethasone can be added to the mixture. These mixtures can be compounded by a local pharmacist. Alternatively, prescription dexamethasone elixir alone, 0.5mg/ ml, can be used as a rinse – one tablespoon for two minutes four times a day – or OTC Rincinol can be used as a rinse to coat the lesions.
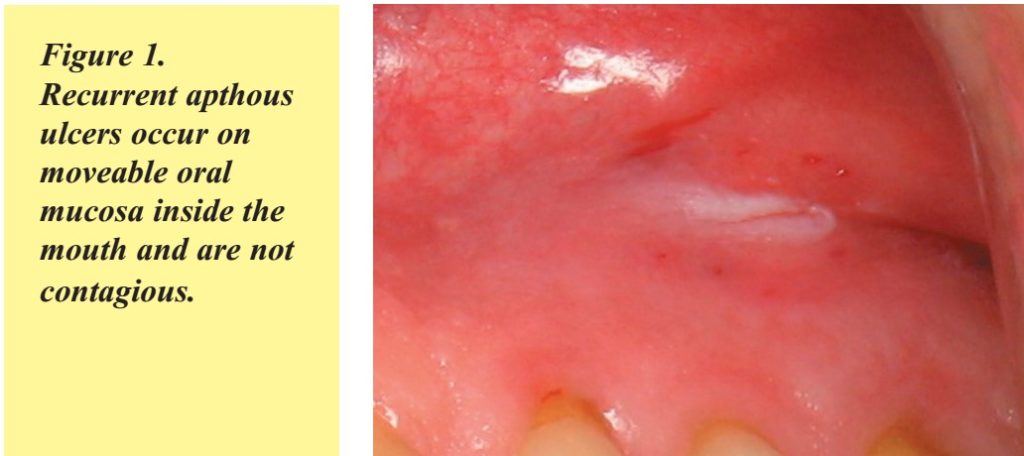
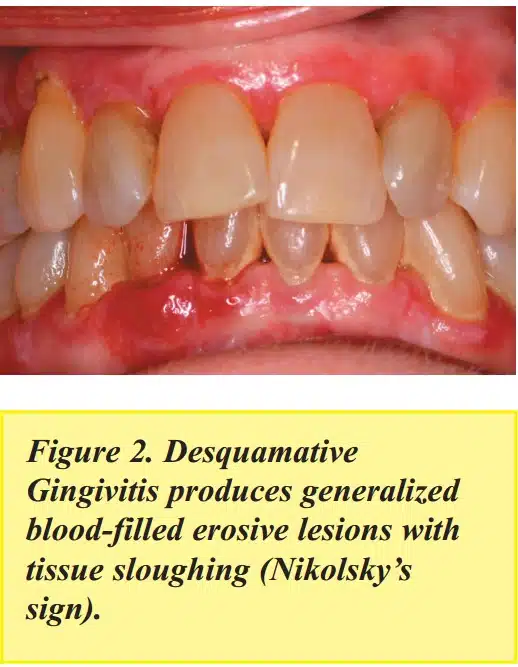
Treating Generalized Painful Ulcerations
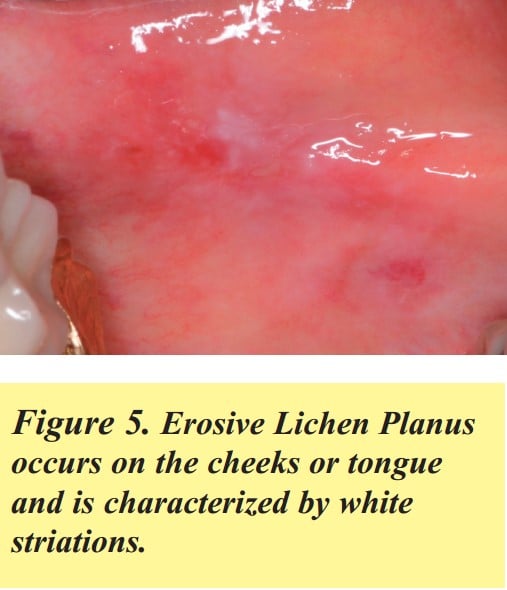
More generalized, or occasionally localized, blood-filled erosive lesions with tissue sloughing (Nikolsky’s sign) sometimes form on the gums and cheeks. These are usually caused by Desquamative Gingivitis (Benign Mucous Membrane Pemphigoid). Generalized or localized painful erosive lesions on the cheeks or tongue characterized by white striations are caused by Erosive Lichen Planus. These are both considered autoimmune diseases, and treatment is palliative, and not curative.
Treatment: An anti-oxidant gel called PerioSciences AO ProVantage Antioxidant Gel can be applied five times a day for mild cases. For more severe cases, a steroid gel called Clobetasol 0.05% (15gm tube) can be prescribed and applied with a Q-tip twice daily. Alternatively, dexamethasone elixir 0.5mg/ml (12 oz. bottle) can be used as a rinse, one tablespoon for two minutes four times per day. In severe cases, this rinse can be used in combination with Clobetasol gel. For Desquamative Gingivitis, doxycycline 100 mg once a day for 30 days has been found very useful.
These conditions are sometimes a painful annoyance but they are not serious and recurrence is common. If not painful, no treatment is needed.
However, in addition to the treatments mentioned above, maintaining good oral hygiene is crucial in managing generalized painful ulcerations. This includes regular brushing, flossing, and using mouth rinses to keep the mouth clean and reduce the risk of bacterial infections.
It’s also important to not consume spicy foods, acidic foods, and hot food that may further irritate the oral mucosa and exacerbate the condition. Addressing any underlying nutritional deficiency, autoimmune disease, or systemic conditions can also help in managing these painful ulcers.
Treating Primary Herpes Infection
Primary Herpes Infection will sometimes occur, most often in children, but occasionally in adults. This viral infection is characterized by very painful sores throughout the mouth, including the gums and throat. It is often accompanied by fever, swollen lymph nodes, difficulty eating, and fatigue. The outbreak usually lasts from seven to 14 days and then goes away on its own. It is a very painful, but not a serious condition. It is contagious during the outbreak.
Treatment: prescription Valtrex, 500 mg, take two caplets twice daily for five days. Treatment with the so-called “Magic Mouthwash” containing Benadryl, Maalox, and viscous xylocaine will reduce pain dramatically. Chloraseptic spray can numb the tissue before eating.
Treating Pemphigus Vulgaris
Pemphigus Vulgaris causes more serious, diffuse, very painful ulcerations throughout the mouth, and on the skin, and requires a special immunofluorescent biopsy to diagnose. Fifty percent of patients with this condition present first with oral lesions before the onset of skin lesions resembling a burn.
Treatment: This is a serious medical condition and requires management by a dermatologist, often with systemic steroids.
Treating Yeast Infections
Sores on the corners of the mouth are called Angular Cheilitis and cause pain when opening and closing the mouth. These sores are usually caused by oral candidiasis, a yeast fungal infection (Candida albicans) secondary to wear or loss of teeth. The loss of teeth, in turn, causes overclosure of the mouth, creating a crease at the corners of the mouth where saliva accumulates.
At times, yeast infections such as oral candidiasis can be a result of various risk factors, including poor oral hygiene, dry mouth, systemic corticosteroids, radiation therapy, or certain health conditions like diabetes.
Regular oral examinations and clinical examinations are important in monitoring the progress of the infection and ensuring that any complications, such as oral leukoplakia or other mucosal lesions, are detected and treated promptly.
In some cases, treatment options may include topical therapy, systemic therapy, or surgical excision, depending on the severity and clinical presentation of the infection.
Treatment of Angular Cheilitis
Each patient should avoid touching the area with their tongue. They should keep the corners of their mouth dry by dabbing frequently with facial tissue. Prescription Mycolog-II ointment is then applied four times a day until healing occurs. Alternatively, OTC Monostat 7 vaginal cream can be applied four times a day.
Inside the mouth, yeast infection is usually characterized by white patches that often can be scraped off. Occasionally, it shows up as red patches, or as a black, hairy tongue. This oral infection is usually caused by prolonged antibiotic use, steroid inhalants, or lowered immune system.
Treatment of yeast infections inside the mouth: Mycelex troche (clotrimazole) 10 mg allowed to dissolve in the mouth five times a day for 14 days. An alternative is Nystatin oral suspension (100,000 units/ ml-dispense 240 ml), take one teaspoon and swish for two minutes, then swallow, four times a day. For more severe yeast infections, Diflucan 100 mg can be prescribed — 15 tablets, take two tablets, then one tablet daily for 13 days.
Besides the treatments mentioned above, maintaining proper oral hygiene and addressing any underlying health conditions is crucial in managing Angular Cheilitis. Dry mouth, poor nutrition, and certain systemic conditions like diabetes can contribute to the development of this painful sore. It is essential to keep the mouth clean by using mouth rinses, brushing regularly, and using a tongue scraper to remove bacteria and debris.
In some cases, a bacterial infection may be present, requiring a targeted approach using appropriate antibiotics. Regular dental treatment and oral examinations are essential in managing this condition and preventing complications.
Diagnosing Oral Cancer
Lesions that may be oral cancer include a mouth ulcer that doesn’t heal, a lump that does not go away, a white patch anywhere in the mouth, difficulty swallowing, or a swollen lymph node in the neck. The gold standard is to biopsy any suspicious lesion. Sometimes, a special fluorescent light can be used to help screen for cancer and determine if a biopsy is indicated.
Risk factors for oral cancer are smoking, excessive alcohol consumption, and especially chewing tobacco or snuff. Chewing tobacco increases the risk of oral cancer by a staggering 50 times. Stopping any of these habits will substantially reduce the risk of oral cancer.
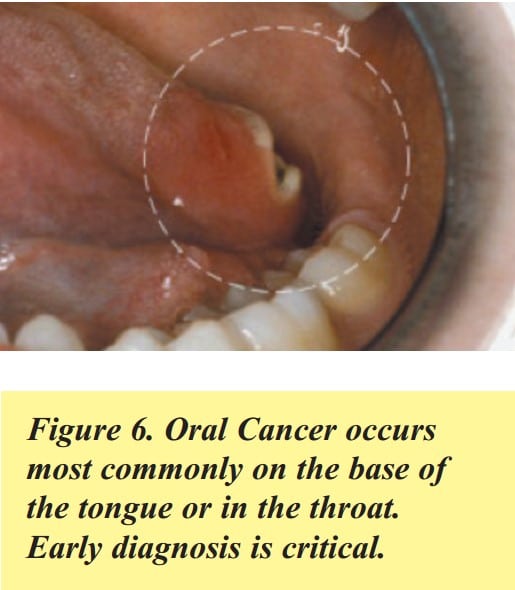
An emerging risk factor is Human Papillomavirus (HPV16) infection, a sexually transmitted virus that is causing throat cancer in younger people. Testing positive for HPV16 means you are at greater risk of throat cancer and need to be monitored more closely. These cancers occur most commonly on the base of the tongue or in the throat, so these areas need to be examined thoroughly during an oral cancer examination. A simple salivary DNA test can determine if a patient is HPV-positive. The Centers for Disease Control recommends that all boys and girls between the ages of 12 and 26 be vaccinated against HPV16, ideally prior to sexual exposure to the virus.
Oral cancer kills more people annually than cervical or prostate cancer. Oral cancer has only a five percent survival rate at five years. If found early, survival increases dramatically, so any suspicious lesion should be examined, and possibly biopsied, as soon as noticed.
Drugs Used to Treat Osteoporosis and Bone Cancer Which May Cause Osteonecrosis of the Jaws
The many bisphosphonates and monoclonal antibodies which are used to treat osteoporosis and bone cancer often cause osteonecrosis of the jaws. As dental clinicians, it is important that we are aware of this side effect before treating our patients who are taking these drugs. The tables below summarize these drugs, the route these drugs are administered, and their likelihood of causing osteonecrosis of the jaws as reported by Dr. Robert Marx at the University of Miami Division of Oral and Maxillofacial Surgery.
Drugs Used to Treat Osteoporosis
Osteoporosis is a condition in which the bones become weak and brittle, increasing the risk of fractures. Bisphosphonates are a class of drugs commonly used to treat osteoporosis. Examples of bisphosphonates include alendronate (Fosamax), risedronate (Actonel), and zoledronic acid (Reclast). These medications can help slow down bone loss and reduce the risk of fractures.
| Drug | Classification | Action | Dose | Route | % of Reported Cases of Osteonecrosis |
|---|---|---|---|---|---|
| Alendronate (Fosamax Generic) | Bisphosphonate | Osteoclast Toxicity | 70 mg/wk | Oral | 82% |
| Residronate (Actonel Atelvia) | Bisphosphonate | Osteoclast Toxicity | 35 mg/wk | Oral | 1% |
| Ibandronate (Boniva) | Bisphosphonate | Osteoclast Toxicity | 150 mg/mos | Oral IV | 1% |
| Zoledronate (Reclast) | Bisphosphonate | Osteoclast Toxicity | 5 mg/yr | IV | 6% |
| Denosumab (Prolia) | Monoclonal Antibody | Osteoclast Impairment | 60 mg/6 mos | Subcutaneous | 10% |
Teriparatide (Forteo) and raloxifene (Evista) are also used to treat osteoporosis but work differently, so they don’t cause osteonecrosis, and no special precautions are necessary.
Drugs Used to Treat Bone Cancer
Bone cancer can be treated using various medications, such as monoclonal antibodies. Denosumab (Xgeva) is an example of a monoclonal antibody used to treat bone cancer. It works by targeting and inhibiting a protein that helps cancer cells grow and spread in the bone.
Both bisphosphonates and monoclonal antibodies can potentially cause osteonecrosis of the jaws. This condition involves the death of bone tissue in the jaw, leading to pain, swelling, and exposed bone. If you are taking any of these medications and require dental treatment, it’s essential to inform your dental clinician to ensure appropriate precautions are taken.
| Drug | Classification | Action | Dose | Route | % of Reported Cases of Osteonecrosis |
|---|---|---|---|---|---|
| Zoledronate (Zometa) | Bisphosphonate | Osteoclast Toxicity | 4 mg/mo | IV | 67% |
| Pamidronate (Aredia) | Bisphosphonate | Osteoclast Toxicity | 90 mg/mo | IV | 18% |
| Bevacizumab (Avastin) | Monoclonal Antibody | VEGF Inhibitor | 100-400 mg/ 14 days | IV | <1% |
| Sunitinib (Sutent) | Tyrosine Kinase Inhibitor | Osteoclast Toxicity | 5 mg/yr | IV | <1% |
| Denosumab (Xgeva) | Monoclonal Antibody | Osteoclast Inhibitor | 120 mg/mo | IV | 15% |
When using drugs to treat bone cancer, it is crucial to consider the potential impact on oral health and the possible development of oral infections or conditions.
Oral hygiene, mouth rinses, and regular dental treatment are essential in maintaining oral health while undergoing cancer treatment, as radiation therapy and certain medications may cause dry mouth, which can contribute to the development of oral infections and mucosal lesions.
Additionally, cancer treatments may lead to nutritional deficiencies or exacerbate existing autoimmune diseases, increasing the risk of oral complications.