Diagnosing and Treating Drug-Induced Osteonecrosis of the Jaw, and TMJ and Tooth Pain
Preventing and treating necrosis of the jaw resulting from drugs taken for osteoporosis is an important consideration for today’s clinicians in determining the appropriate dental care.
As our patient population ages, more and more patients, especially females, are taking drugs for osteopenia and osteoporosis. These drugs impair osteoclastic bone resorption, and therefore bone renewal, thereby retaining old bone and reducing its ability to turn over.
Because the alveolar bone in the jaws turns over faster than any other bone in the adult skeleton, it is the focal point for drug-induced osteonecrosis of the jaws (DIONJ). This condition is especially important when considering extractions, osseous surgery and the placement of dental implants.
The following discussion is summarized from a Position Paper on Drug- Induced Osteonecrosis of the Jaws (DIONJ) by Robert E. Marx, DDS, and Ramzey Tursun, DDS, University of Miami Division of Oral and Maxillofacial Surgery, September 27, 2016.
The current drugs that place osteopenia and osteoporosis patients at risk for DIONJ are the oral bisphosphonates, alendronate (Fosamax and generic equivalents), residronate (Actonel and Atelvia) and ibandronate (Boniva); the subcutaneously- injected denosumab (Prolia and Xgeva); and the intravenous bisphosphonate zoledronate (Reclast and Zometa.)
Of the oral bisphosphonates, alendronate (Fosamax) is the drug linked to 96 percent of cases of DIONJ compared to three percent of cases caused by residronate (Actonel) and one percent of cases caused by ibandronate (Boniva). This is mostly due to the fact that alendronate is marketed at twice the dose of all other bisphosphonates (70mg/week), while it has the same absorption, distribution, and the same potency as the others.
Although zoledronate as Reclast is relatively new, and only 5mg is delivered by IV only once yearly for osteoporosis, it is causing several cases of DIONJ. This is because the half life in bone of 11 years is the same for all the bisphosphonates, and the IV infusion loads the bone 140 times more than any oral bisphosphonate.
Therefore, dental professionals must realize that, although some DIONJ cases may occur sooner, the significant DIONJ risk for an oral bisphosphonate begins at about three years of weekly dosing, and with IV Reclast at about the fourth yearly dose.
Those osteopenia/osteoporosis patients converted to Reclast after taking an oral bisphosphonate are at risk for DIONJ before the fourth dose, and may need a drug holiday longer than nine months.
The FDA has recommended that no one needs to take a bisphosphonate for more than five years.
Denosumab (Prolia and Xgeva) as a RANK ligand inhibitor does not seem to bind to bone or accumulate in bone as do bisphosphonates, and has a half life in bone of 26 days. Therefore, if this drug has been taken for less than three years, discontinuation with a shorter drug holiday of three months is adequate.
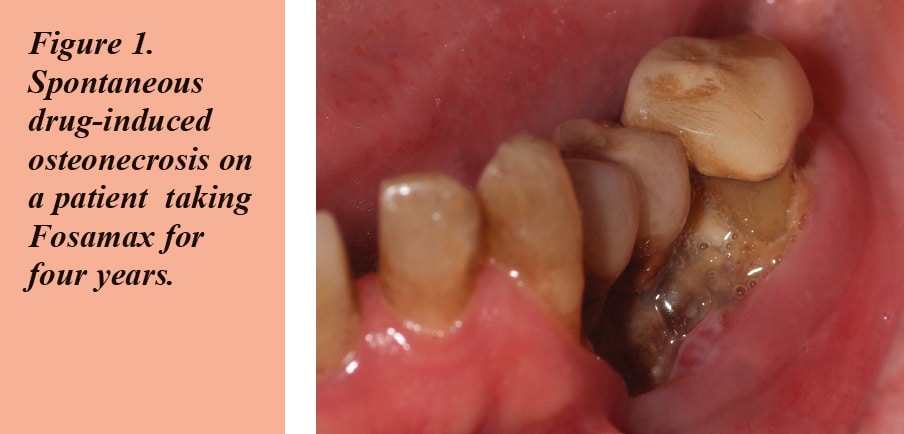
Switching from a bisphosphonate to denosumab causes necrosis relatively frequently and should be avoided.
Discussions with the patient’s physician about the choice of medicine and dosage is very important.
See the Spring 2017 issue of The PerioDontaLetter for a table summarizing the many bisphosphonates and monoclonal antibodies which are used to treat osteoporosis and bone cancer. The table includes the route these drugs are administered, and their likelihood of causing drug-induced osteonecrosis of the jaw.
Patients on IV bisphosphonates for the treatment of cancer are at much greater risk of DIONJ than patients taking oral bisphosphonates.
Prevention – What to Do and What Not to Do
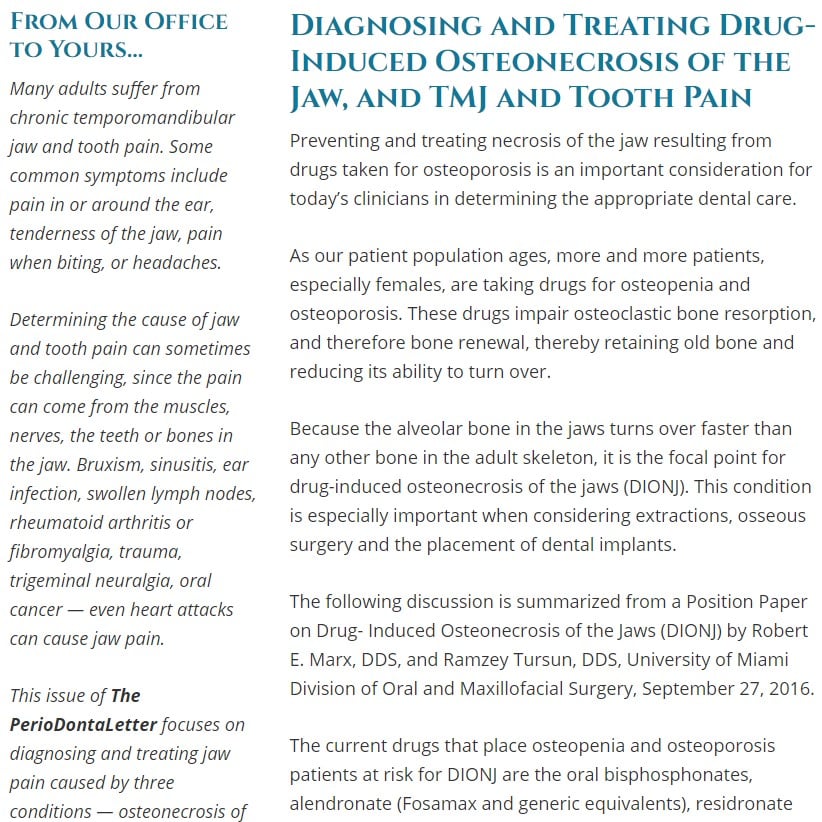
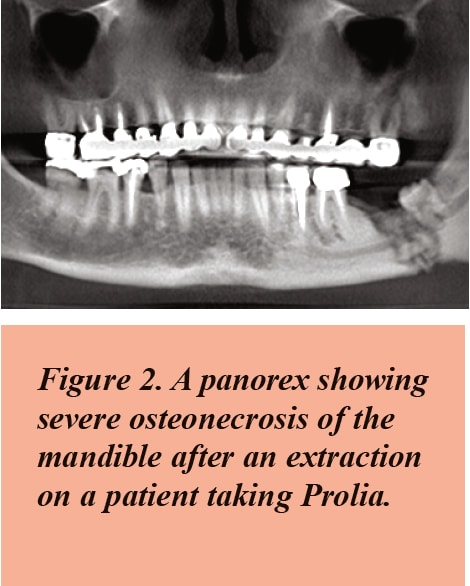
The initiating event for DIONJ is surgery involving the alveolar bone: tooth removals (62%), osseous periodontal surgery (5.6%), dental implants (2.2%), bone biopsy (1.1%), and apical resective endodontic therapy (0.5%) with 29% spontaneous development (more commonly from the higher IV doses used to treat bone cancer patients). Occlusal trauma can also be a factor in lower lingual necrosis.
For those patients requiring bone surgery who are taking an oral bisphosphonate, it may be reasonable to assess the bone turnover suppression by requesting a morning fasting serum c-terminal telopeptide (CTX test). (Many experts have questioned the usefulness of this test.) A value of 150 pg/ ml or greater is consistent with bone healing, if the test is not invalidated by cancer, steroids or methotrexate.
When the CTX test is above 150 pg/ml, the planned alveolar bone surgery can be accomplished and a three-month drug holiday requested from the prescribing physician to cover the healing period. If the CTX value is below 150 pg/ml, a drug holiday prior to performing alveolar bone surgery, placing implants, or orthodontic treatment is advisable.
For patients who have taken an oral bisphosphonate for more than three years, the initial CTX is usually below the 150 pg/ml level. For such patients, a longer drug holiday is usually necessary. Many are required to be as long as nine months or more.
Treating DIONJ in the Osteopenia/ Osteoporosis Patient
Exposed bone represents necrotic bone. If the offending drug is continued, the area of exposed bone is likely to increase, and secondary areas of exposed bone may develop. It is advised to request a drug holiday from the prescribing physician.
Studies have shown that a drug holiday of nine months will result in a spontaneous sequestration and exfoliation of the exposed bone, followed by mucosal healing in 50 percent of cases. These cases are usually the smaller areas of exposed bone. During this drug holiday, use 0.12 percent chlorhexidine oral rinses three times daily to prevent secondary infection.
If secondary infection develops, penicillin VK 500mg QID, or doxycycline 100mg once daily, are the best antibiotics to use. For larger areas of osteonecrosis, referral to an oral surgeon is indicated.
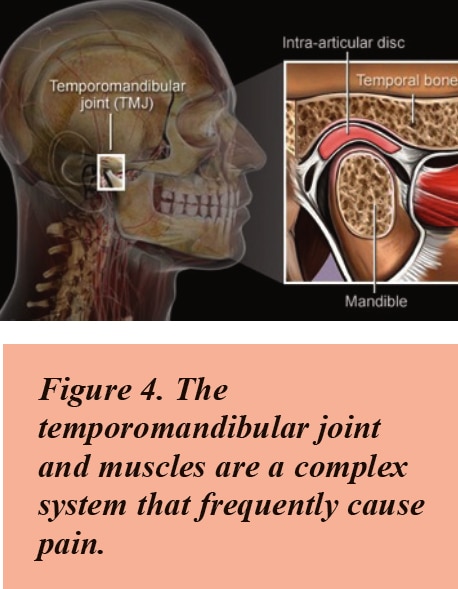
Treating Temporomandibular Joint Dysfunction
Pain in the jaw when opening and biting may involve the temporomandibular joint (TMJ) and surrounding muscles. It usually involves spasm in the muscles that open and close the mouth. Pain in these muscles is like a strained muscle in other parts of the body and is treated similarly.
The following self-management steps may provide some relief for most TMJ muscle pain.
- Cold packs can be applied on the sore muscle or joint when the pain is acute. If the pain is chronic, hot packs can be applied for 15 minutes on and 15 minutes off for two hours once or twice each day as long as pain continues.
- Patients can rest jaw muscles by eating soft foods, avoiding chewing gum and clenching their teeth. If patients clench, have them put their lips together, teeth apart and take two deep breaths to relax.
- Advise patients not to open their jaws wide, and to limit their jaw opening when yawning.
If relief is not obtained, professional assistance will likely be required.
- An occlusal bite plane can be constructed to help the patient relax the jaw muscles and significantly contribute to the diagnosis of the etiology. Patients can wear the bite plane at night if discomfort is mild. For more severe pain, a bite splint can be worn for 24 hours each day to help bring relief. The use of this intraoral appliance may permit the muscles of mastication to relax and diminish the muscular spasms.
- If it is determined that occlusal factors are contributing to the TMJ pathology and symptoms, changes in the occlusion by occlusal equilibration and/or orthodontics may be indicated.
- Anti-inflammatory medications like naproxen or ibuprofen can help relieve pain.
- For acute pain, a muscle relaxant similar to Robaxin can be prescribed (two 500mg tablets four times a day) to help reduce the spasms and discomfort.
- If the pain is severe or not relieved by these steps, referral to a dentist who has expertise in TMJ treatment may be considered. Additionally, TMJ images should be considered to rule out other causes of the patient’s symptoms and to help diagnose the etiology of the discomfort.
Diagnosing and Treating Tooth Pain
A symptomatic tooth may have pain of pulpal and/or periodontal origin. The nature of that pain is the first clue in determining the etiology of such a problem.
Radiographic and clinical evaluation is essential in arriving at the diagnosis.
Careful history taking and examination are essential to an accurate diagnosis.
Cracked Teeth
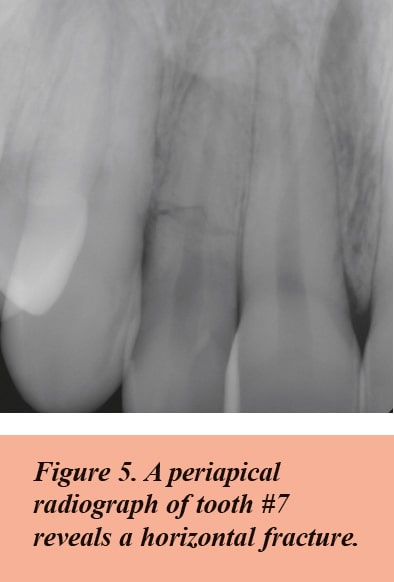
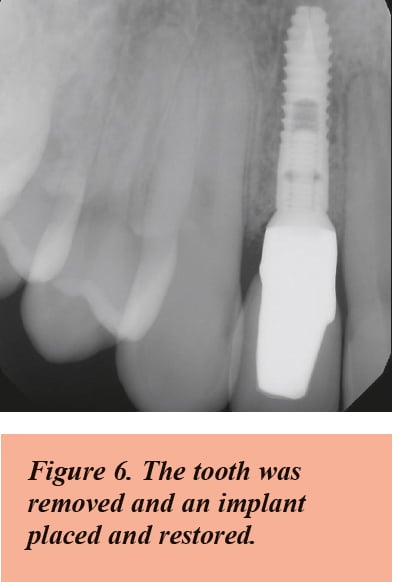
If the pain is sharp when biting and lasts only a few seconds, the patient may have a crack in the tooth. If the crack is confined to the coronal aspect of the tooth, the tooth can often be saved without endodontic therapy and with a full coverage restoration. If the crack involves the pulp, the problem is often resolved with endodontic and restorative therapy. Crown lengthening below the fracture line and a full coverage restoration will usually resolve the problem. If the tooth has a large crack or a vertical root fracture, it will usually have to be extracted and replaced by an implant or bridge.
Endodontic Treatment
If the pain is severe or sharp, keeps the patient up at night, and is exacerbated by thermal changes lasting more than 15 seconds, it most likely means the pulp of the tooth is dying and the patient will need endodontic treatment. Other indications that the tooth may need endodontic treatment include pain on biting, pain when the apex of the root is palpated, and pain in the region of the ear.
If prior endodontic treatment has been completed and pain returns, endodontic retreatment or endodontic surgery may be considered. If these approaches are not successful, the tooth may need to be extracted and replaced by a fixed prosthesis or an implant.
Periodontal Problems
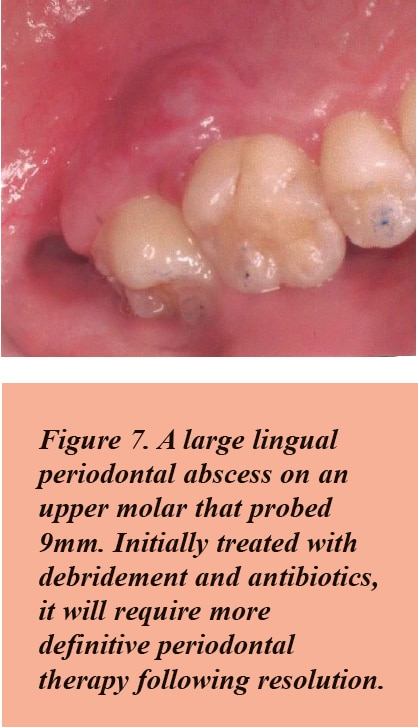
If the pain is dull and less severe, periodontal etiology should be considered. Usually the patient can identify the specific location of the pain in contrast to pulpal pain which can be difficult to localize. Exudate and pocket depth of at least 5mm or more is usually present.
Periodontal therapy with debridement, irrigation, and topical antibiotics will usually manage the acute infection. For larger infections, systemic antibiotics are often needed. Later, conventional periodontal therapy is usually required.
Root Sensitivity
If the pain is made worse by thermal changes lasting only a few seconds without pain on mastication, the source may be root sensitivity. Root sensitivity can be treated by desensitizing medications.
Conclusion
Because of the complexity of these infections, an interdisciplinary approach with good collaboration between the periodontist, the restorative dentist, and the endodontist is critical to achieving the correct diagnosis and determining the appropriate treatment for jaw pain caused by these three conditions.
Causes and Treatment of Root Sensitivity
One of the main causes of root sensitivity is eating lots of fruit or drinking fruit juices. Fruit is obviously good for us, but it also causes lots of cavities and root sensitivity.
Most fruits are very acidic and contain lots of fructose. The acids in fruits are responsible for much of the root sensitivity that we see.
Other acidic causes of sensitivity are vinegar, yogurt, sports and soft drinks, and tea. Check the patient’s diet closely for acidic content if they are experiencing root sensitivity.
These acids open up dentinal tubules in the root and allow cold, hot or touch stimuli a pathway into the pulp of the tooth causing pain. The pain is usually short lived.
If the pain lasts for more than a few seconds, the pulp may be infected and endodontic treatment may be indicated.
Drinking acidic beverages through a straw, and eating and swallowing fruits quickly will minimize acidic exposure to tooth roots. Rinsing with water immediately after ingesting will dilute the acidic effect.
Patients should wait to brush for at least 30 minutes as the acids soften the roots, making them more susceptible to wear notching and cemental abrasion.
Sipping acidic drinks is especially damaging by keeping acid on the root. Drinking quickly reduces the time of acid demineralization so advise your patients: “gulp don’t sip” to reduce sensitivity.
The fructose in fruits is closely related to sucrose (sugar). It will cause cavities just like all sugar products, including and especially Altoids, Tic Tacs, and other sugar-containing breath mints.
To help control sensitivity, patients can use toothpastes containing potassium nitrate and fluoride like Sensodyne, and rinse with fluoride rinses like Act Complete.
Over-the-counter Sensi-Strips can be applied daily for ten minutes to block the tubules with oxalate crystals. More potent prescription fluoride pastes are available which will protect roots and also reduce caries.
In the office, fluoride varnish can be applied. Even more effective are lightcured coatings performed in office with Vanish XT or Seal and Protect.
If root sensitivity continues to be a problem, periodontal therapy may be possible to re-cover the exposed roots.
If root coverage is not possible, the sensitive area can be bonded. In rare cases, endodontic therapy may be required to resolve the sensitivity.