
major etiological factor for periimplant mucositis. Peri-implant mucositis develops due to an imbalance between the bacterial challenges of the microbial biofilm and the local host response. Evidence suggests that periimplant mucositis can be successfully and predictably treated, and is reversible if caught early. Peri-implant mucositis has been identified as a precursor to peri-implantitis.
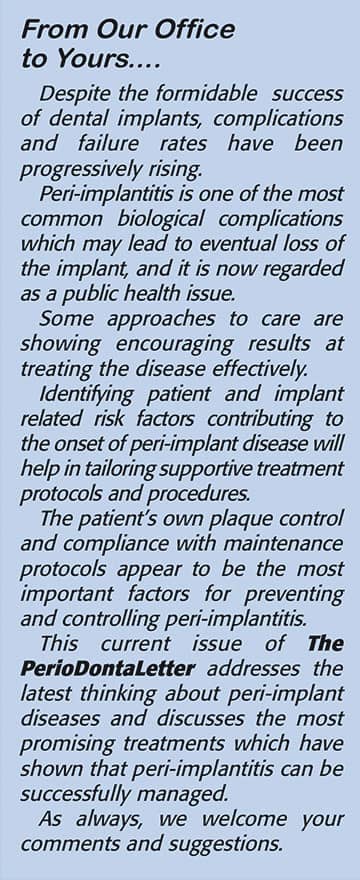
Peri-implantitis is a plaqueassociated pathological condition occurring in dental implant supporting tissues characterized by inflammation in the peri-implant tissues and subsequent progressive radiographic loss of supporting bone.
Other clinical signs are bleeding on probing, increased probing depths, suppuration, and possibly recession of the gingival margin around the crown.
Peri-implantitis usually requires surgical treatment to prevent progressive bone loss and/or implant failure.
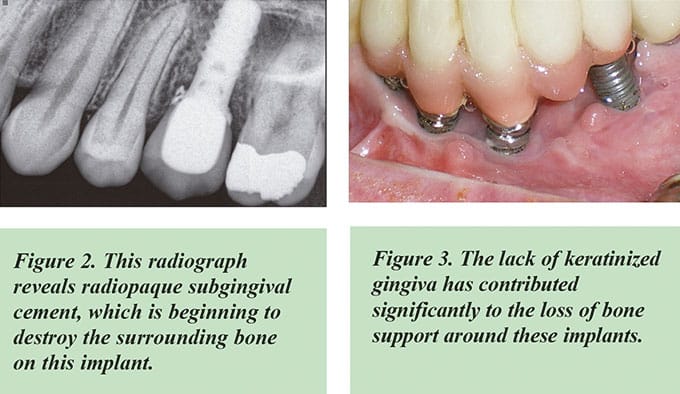
The principal factors for recession of the peri-implant mucosa around the crown margins are loss of supporting bone, thin gingival biotype (phenotype), lack of keratinized tissue, loss of attachment on adjacent teeth, and sometimes facially-positioned implants.
Several studies have suggested that as many as 80 percent of patients will develop peri-implant mucositis, and as many as 40 percent of implants and
18.5 percent of patients will develop peri-implantitis. An even greater frequency of peri-implant diseases was recorded for smokers, diabetics, excessive luting cement, and individuals with active periodontal disease elsewhere in the mouth.
One study following 2,300 implants for ten years found that the risk of implant failure was eight times greater in patients with severe periodontal disease than in patients with healthy supporting tissue and bone.
When compared with healthy implant sites alone, peri-implantitis is associated with a higher percentage of anerobic bacteria — the same bacteria which cause periodontitis.
Preventing
Peri-Implant Disease
It appears that both the clinicians who place the implant and those who restore it can mitigate some of the risk factors for peri-implant disease.
The surgical placement should be as ideal as clinically possible. Adequate bone volume (reconstructed if indicated), appropriate diameter of the implant fixture relative to the bone anatomy, and depth and angulation of the implant will minimize restorative complications. A prosthetically-driven treatment plan is imperative for a predictable outcome.
• The patient must be able to adequately clean the restoration with an oral hygiene device such as an interproximal brush. The embrasure space simplifies access for enhanced plaque control.
• Pontic areas should be convex rather than concave to ensure
cleansability.
• The peri-implant tissues should be monitored for early indications of disease. Treatment should begin immediately to prevent the development of peri-implantitis associated with bone loss.
• A radiograph should be taken annually or every other year to monitor for crestal bone loss changes suggesting the onset of a peri-implantitis lesion.
Patient selection prior to dental implant consideration is important in minimizing the risk of future periimplant complications. Patients with active and previously treated periodontitis have a higher risk of periimplantitis. In addition, many studies indicate that patients with diabetes or a smoking habit also will have a higher risk of peri-implantitis.
The role of periodic supportive periodontal maintenance (SPT) for patients with dental implant restorations has been shown to be very effective in addressing inflammatory issues and monitoring crestal bone levels compared to those patients without supportive periodontal maintenance.
Research has found patients who regularly comply with periodontal maintenance, with a minimum recall interval of five to six months, experience significantly reduced associations with peri-implant mucositis (-55%), marginal bone loss (-34%) and peri-implantitis (-77%).
Alveolar bone and soft tissue deficiencies may occur following extractions and healing without alveolar ridge preservation. When extracting teeth, every precaution should be taken to preserve and regenerate hard and soft tissue to provide an optimum site.
Compromised implant sites will often require augmentation procedures to provide a better esthetic and functional outcome for the patient.

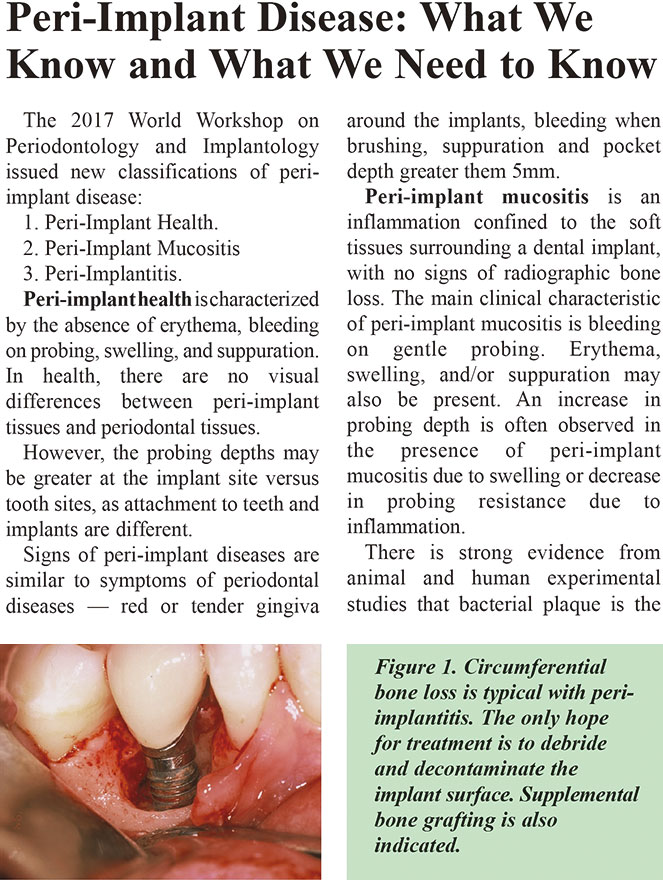
The risk of peri-implant disease is substantially greater with cemented restorations compared to screwretained restorations.
• Residual cement must be removed when placing a cement-retained restoration. Cement provides a favorable platform for plaque deposition, much like calculus on a tooth. The onset of inflammatory signs and suppuration can take years to develop and is often not discovered until there is substantial loss of attachment.
• The cementation process can be well controlled by using a duplicate (mock) abutment inserted into the crown. This allows all excess cement to be extruded and removed prior to permanent cementation.
• Cements which are radiopaque should be used rather than those that are radiolucent in order to identify the possible presence of excess cement on a radiograph.
• The soft tissues adhere to an abutment surface via a fragile hemidesmosomal attachment. This soft tissue attachment can be readily disrupted by excess cement flow.
Implant
Considerations
In health, the soft tissues attached to the implant collar and abutment have a weak epithelium hemidesmosomal attachment, or a connective tissue attachment. This attachment is the first line of defense against inflammatory changes of peri-implantitis.
Numerous research publications and clinical case reports have described the different soft tissue attachment responses to various implant collar, implant and abutment surfaces (smooth metal, roughened, microtextured or ceramic).
Shapoff and others have demonstrated in case reports successful, long-term clinical outcomes utilizing microtextured implant technology.
Custom abutments have generally become the treatment of choice. These permit the design of the abutment/crown interface to be well-controlled just .5-1mm subgingivally allowing for efficient cleansability.
Screw-retained restorations virtually eliminate the problems associated with cement-retained restorations. The implant industry is developing new, innovative designs which simplify screw-retained restorations.
The evidence strongly supports the benefits of a thick gingival biotype and an adequate zone of keratinized gingiva on the long-term health of the periimplant tissues. Keratinized gingiva may also have advantages regarding patient comfort and ease of plaque removal.
Diagnosing
and Treating
Peri-Implant Diseases
Probing of peri-implant tissue with light force has been etermined to be a safe and important part of a complete examination.
Peri-implant mucositis is a reversible condition and requires immediate intervention to treat and prevent further deterioration.
Thorough mechanical debridement of the area along with improved plaque control and local anti-microbials such as
Betadine or chlorhexidine irrigation is often sufficient to resolve peri-implant mucositis. Cervitec Plus, a chlorhexidine and thymol varnish, has been used.
Using a water irrigator with chlorhexidine has been shown to reduce peri-implant mucositis by up to 70%.
Some practitioners have found air polishing with glycine powder effective at removing plaque from dental implants.
The onset of peri-implantitis may occur early following implant placement.
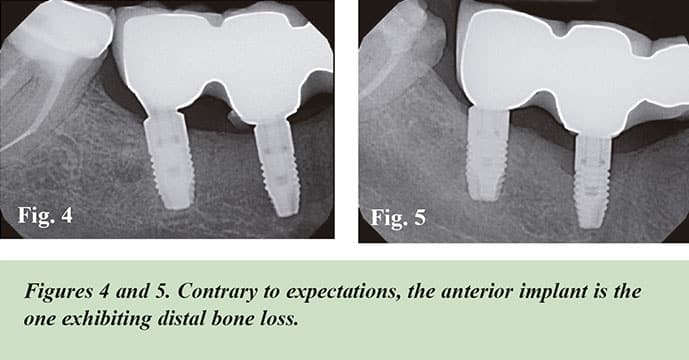
Radiographic bone level loss of 3mm or greater, and probing depths of 6mm or more, indicate peri-implantitis.
Peri-implantitis, in the absence of treatment, seems to progress in a nonlinear and accelerating pattern. The tissues supporting an implant are more vulnerable to periodontal pathogens than teeth. Most implants lack a connective tissue attachment to the implant collar. Once infection starts, these implants are much more vulnerable to disease progression than natural teeth, which do have an attachment to the cementum. The loss of attachment and bone support around an implant tends to be circular, rather than vertical, as it is with natural teeth.
Nonsurgical
Treatment
Currently, the only proven way to stop the progress of peri- implantitis is mechanical debridement to remove the bacteria and their byproducts, and/or eliminating sub gingival excess cement at the abutment/implant margin.

The use of antimicrobial oral rinses, irrigation, and local drug delivery systems has been shown to have a limited beneficial adjunctive effect on periimplantitis when used in combination with mechanical debridement. If nonsurgical therapy has been attempted and the inflammation has not resolved, surgical therapy is required.
Surgical Treatment
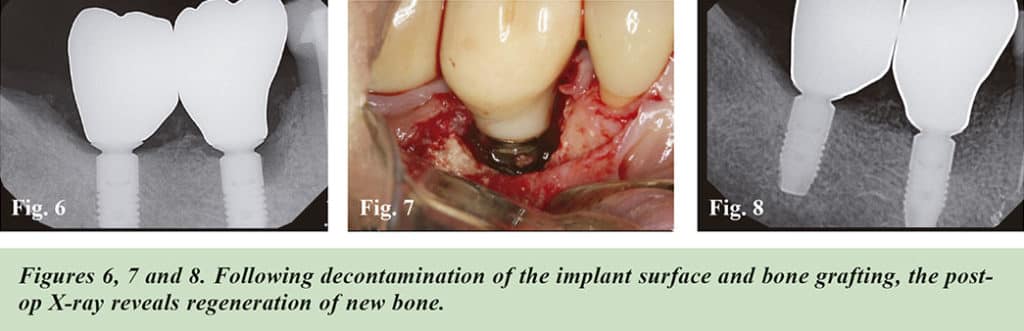
A full-thickness flap around the affected dental implant must be elevated to completely visualize the implant surface. The implant can then be mechanically debrided to fully remove any retained cement, the adherent biofilm, or inflamed granulomatous tissue.
Other methods to debride a plaquecontaminated abutment or implant surface include appropriate use of sonic and ultrasonic scalers, lasers, airpowder abrasion, and various chemical solutions such as citric acid, hydrogen peroxide and saline.
Laser Treatment
Some clinicians have reported success in removing infection and even regenerating bone using laser therapy.
The laser has been shown to help mitigate the bacterial infection without apparent damage to the implant itself or the surrounding tissues.
McCawley and Rams found laser treatment on mostly natural teeth and a few implants immediately suppressed putative bacterial pathogens in deep periodontal pockets to below culture detection limits.
A recent publication demonstrated laser treatment was able to increase crestal bone mass around the implant and reduce probing depth, thus permitting resolution of peri-implantitis.
Regenerative
Treatment
The optimal outcome of periimplantitis treatment is regeneration of the lost hard tissue around the implant.
Following successful implant surface decontamination, various bone regenerative techniques utilizing autogenous, allograft or xenographt bone and growth factors (bone morphogenetic proteins (BMPs), recombinant human platelet-derived growth factor (rPDGF), autologous platelet-rich fibrin (PRF) and barrier membranes) have been used to rebuild lost bone support around the “ailing” implant.
Conclusion
Current knowledge suggests that peri-implant disease is a condition that, while having several traits in common with periodontal disease — in particular the Porphyromonas gingivalis bacteria which causes it — is probably much more complex, and with unique and distinctive features that need to be thoroughly investigated.
Control of periodontal disease in other areas of the mouth prior to implant placement is critical to preventing cross-infection of the implant. Poor plaque control and lack of regular maintenance constitute major risk factors for peri-implantitis.
Strict adherence to regular periodic maintenance is the most important preventive measure, permitting early detection of peri- implant disease.
Improved methods of cementation technique, shallow subgingival margins with the use of custom abutments, and early and frequent follow-up visits in a shared maintenance approach will minimize the often irreversible effects of peri-implantitis.
Clearly, however, the best approach, as always, is prevention.