John Paul Gallardo, D.D.S., P.A., Periodontics and Implant Dentistry
From Our Office
to Yours….
Research shows patients with progressive attachment loss, invasive subgingival pathogens, or multiple deep pockets may significantly benefit from the use of systemic antibiotics as an adjunct to conventional mechanical therapy.
Furthermore, because the morbidity associated with implant-related complications can be significant, prophylactic antibiotic use is recommended before and after implant placement, as is the proper selection of antibiotics in the treatment of the tsunami of periimplantitis.
This current issue of The PerioDontaLetter discusses the most current protocols for the use of antibiotics in the treatment of periodontal disease. Additionally, we focus on the prophylactic use of antibiotics before and after implant placement to prevent periimplantitis and other implantrelated complications. As always, we welcome your comments and suggestions.
Antibiotic Recommendations Prior to and Following Dental Treatment Have Changed
Antibiotics can contribute to the management of periodontal disease and prevent the incidence of implantrelated complications by eliminating specific pathogens which the patient’s immune system cannot overcome.
Research shows antibiotic treatment can reduce pathogenic bacteria before and/or after many common periodontal procedures. Systemic antimicrobial therapy can be used as an adjunct to mechanical therapy in patients with:
- chronic periodontitis, most beneficially in sites with deep probing depths and continued bleeding upon probing
- aggressive periodontitis
- no response to traditional mechanical treatment
- severe periodontal infection
- compromised immune systems
- before and after dental implant placement to prevent related complications
Antibiotics in Periodontal Therapy
Jorgen Slots summarized the rationale for the use of antibiotics as adjuncts in the treatment of periodontal disease and periimplantitis:
- Pockets harbor many different pathogens with diverse susceptibility profiles.
- Eradication of many subgingival pathogens is not predictable with conventional periodontal therapy.
- Because of the ability of antibiotics to penetrate sites inaccessible to traditional instrumentation, systemic delivery of antibiotics has the advantage of killing bacteria in deep pockets, furcations, bifurcations and trifurcations in the gingival tissue, and at other oral sites such as the tongue, saliva and oral mucosa.
Studies show that neither scaling and root planing nor conventional surgical management predictably eliminates all pathogenic organisms.
Data has shown the recolonization of pockets as early as six weeks after scaling and root planing.
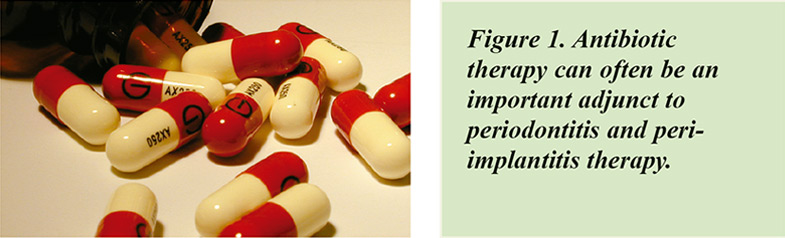
Campylobacter rectus and spirochetes are susceptible to non-surgical scaling and root planing. Porphyromonas gingivalis, Prevotella intermedia, Steptococcus constellatus, Tanneralla forsythia, Fusobacterium, and enteric rods/pseudomonads, Aggregatibacter actinomycetemcomitans or Peptostreptococcus which invade the pocket tissue are resistant to mechanical intervention. (See Figure 2 below.)
Based on research by Berberi et al through August of 2021, the American Academy of Oral Medicine, (AAOM), the ADA in conjunction with the AAOS, and the British Society for Antimicrobial Chemotherapy all advise against the universal use of antimicrobial prophylaxis prior to dental procedures for the prevention of prosthetic joint infections.
The Food and Drug Administration has updated fluoroquinolone labels to warn of the risks of disabling adverse events.
Quinolones — ciprofloxacin, levofloxacin and moxifloxacin — should be severely limited and used only for very specific conditions, such as certain dental infections, sinusitis, bronchitis and urinary tract infections.
The many adverse effects — including the possibility of tendon ruptures and tendonitis; peripheral neuropathy; central nervous system effects, such as psychosis and the exacerbation of myasthenia gravis; and aortic aneurysm/dissection — have been documented to last as long as one and a half years!
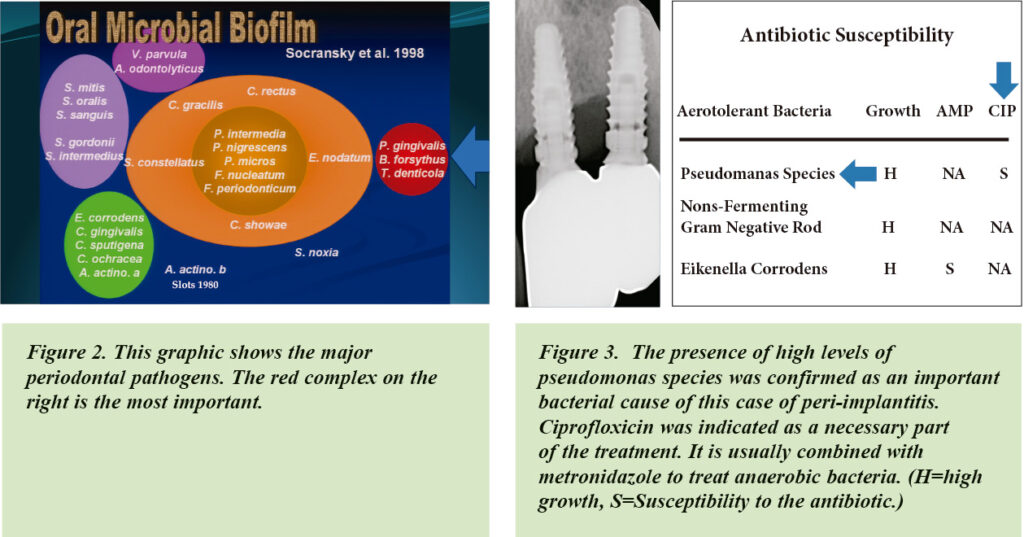
These drugs should be used only in dental patients who culture positive for pseudomonads.
Ciprofloxicin is the oral antibiotic most often used to treat pseudomonads. (See Figure 3 below.)
In one study of 103 implants, gram negative enteric rods/pseudomonas were observed in 47 implants — 46 percent. In this cross-sectional study, probing pocket depth, clinical attachment loss and bleeding on probing were significantly worse on these implants.
Enterococcus faecalis, a virulent pathogen, has occasionally been found to produce localized infection adjacent to teeth and implants along with Pseudomonas aeruginosa suggesting a possible vehicle for the transmission of periodontal and peri-implant disease.
The combination of amoxicillin and clavulanic acid (augmentin) is the best oral antibiotic combination to use in treating enterococcus.
The bacteria found in subgingival biofilm are often resistant to antibiotics. A study of subgingival specimens from deep pockets in 400 adults by Rams et al showed 74 percent were resistant to antibiotics — 55 percent to doxycycline, 43 percent to amoxicillin, 30 percent to metronidazole and 27 percent to clindamycin. Fifteen percent were resistant to a combination of amoxicillin/metronidazole.
Because periodontal pathogens exhibit diverse anti-microbial susceptibility, microbiological analysis is sometimes necessary for proper
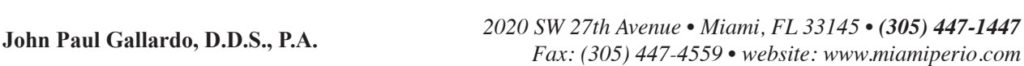
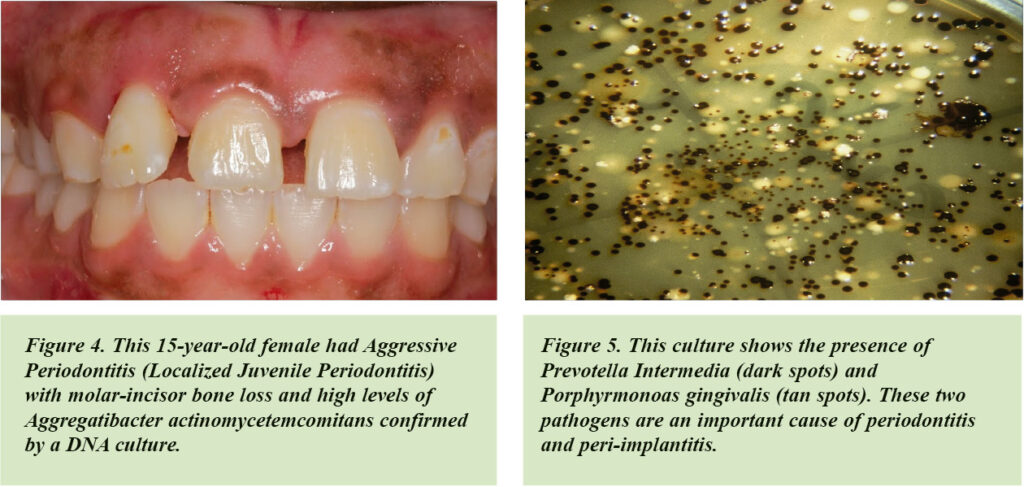
selection of antibiotic therapy. (See Figures 4 and 5 above.)
Gingivitis has been identified as a non-specific bacterial infection. Antibiotics are NOT recommended unless the infection is also associated with systemic disease with existing symptoms, for example, Acute Necrotizing Ulcerative Gingivitis (ANUG) associated with lymphadenopathy.
Antibiotics are unnecessary most of the time, and are only indicated to treat infections of specific bacterial origin. And, to be effective, the pathogen must be susceptible to the chosen medication regimen. An antibiotic strength at least 500 times greater than the systemic therapeutic dose is required to be effective against the bacteria contained in biofilms. For an antibiotic to be effective, the biofilm must first be physically disrupted.
Antibiotic Pre-medication for Patients with Joint Replacement and Cardiac Issues
New guidelines from the American Academy of Orthopedic Surgeons (AAOS) has eliminated the need for prophylactic antibiotics prior to dental treatment for most patients with joint replacements.
In 2017, the AAOS released the appropriate use criteria that identified a very narrow group of patients for whom it would be appropriate to consider using antibiotic prophylaxis.
This cohort includes patients with comorbidities, such as those who are immunocompromised or diabetic, or who have had a previous joint infection.
Prophylactic antibiotics are now recommended only for patients with prosthetic cardiac valves, including transcatheter-implanted prostheses and homografts.
It is also advised for patients with prosthetic materials used for cardiac valve repair, such as annuloplasty rings and chords; for patients with a history of infective endocarditis; and for those with a cardiac transplant with valve regurgitation due to a structurally abnormal valve.
Antibiotics are also recommended for patients with congenital heart diseases — unrepaired cyanotic congenital heart disease, including palliative shunts and conduits. They are recommended for patients with any repaired congenital heart defect with residual shunts or valvular regurgitation at, or adjacent to, the site of a prosthetic patch or a prosthetic device.
Recent evidence suggests that those patients who are at high risk for infectious endocarditis would benefit from antibiotic prophylaxis prior to invasive dental procedures.
Lastly, there is compelling data that the use of prophylactic amoxicillin or ampicillin, but not clindamycin, is effective in reducing both the prevalence and duration of bacteremia following tooth extractions.
Antibiotics in the Prevention of Complications from Dental Implant Placement and Peri-implantitis
Prophylactic antibiotics are recommended to prevent infections when placing implants and bone regenerative procedures. Preoperative and prophylactic antimicrobial medication during the initial healing period from the surgical wound site has been shown to significantly reduce postoperative infections of the soft and hard tissues and decrease failure rates in implant cases.
If however, the goal of treatment is to eliminate a bacterial infection, then antibiotics appropriate to the specific pathogens should be recommended.
Five to seven days of antibiotics are safer and usually just as effective as ten to 14 days. Azithromycin use has been associated with cardiovascular mortality, so should be expressly avoided for patients with arrythmias. It therefore is not indicated for patients taking amiodarone for arrhythmias.
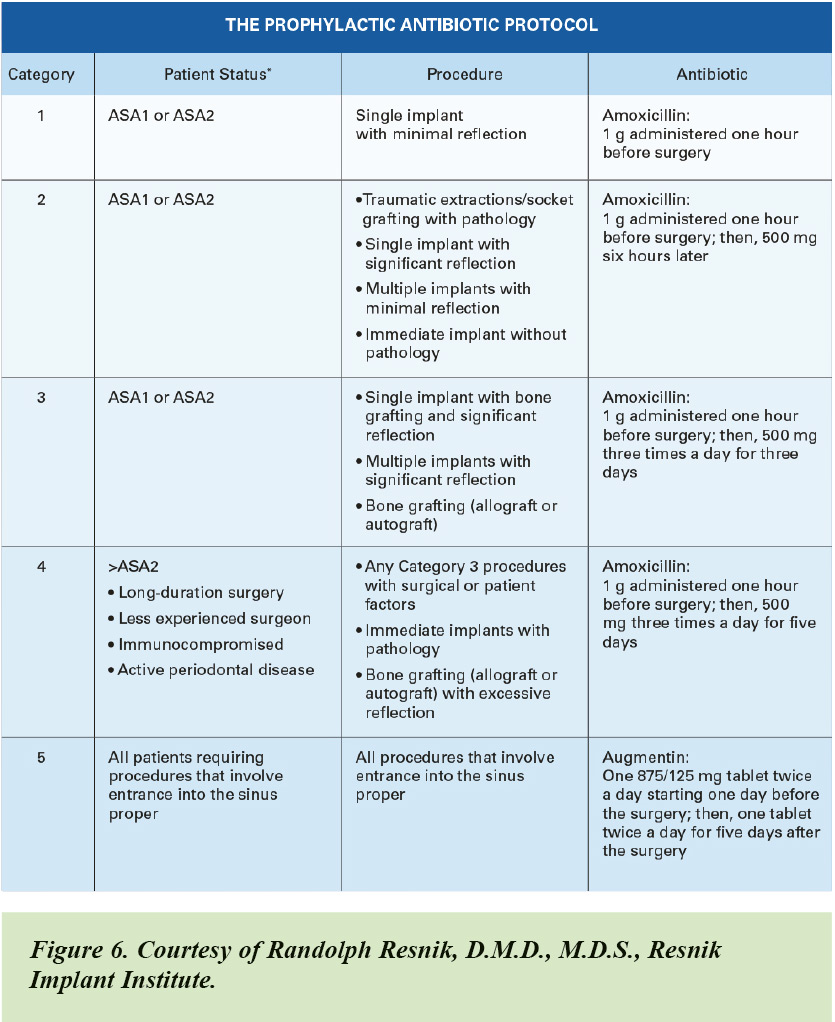
The well-regarded dental surgeon Randolf Resnick recommends the following antibiotics for treating the pathogens known to cause postoperative surgical wound infections in implant and bone grafting surgery: amoxicillin (500 mg), cefuroxime (Ceftin — non anaphylactic allergy to penicillin) (500 mg), and doxycycline (anaphylactic allergy to penicillin) (100 mg).
(See chart with Dr. Resnick’s recommended prophylactic antibiotic protocol for implants.)
Treating Patients Reporting with Allergies to Penicillin
Unfortunately, there have been many poorly conducted studies which have spread false information about allergies to penicillin antibiotics.
Less than one percent of the population is truly allergic to penicillin. About 80 percent of patients reporting a history of allergic reaction have proven not to be sensitive after ten years!
Because of the high rate of selfreporting penicillin allergies, many patients are treated with alternative antibiotics (such as clindamycin phosphate), which predisposes patients to an increased number of complications.
While clindamycin is the most commonly used alternative antibiotic for patients who report a penicillin allergy, studies have associated it with a fourfold increase in surgical site infection compared with the use of beta-lactam (penicillin) antibiotics.
It is no longer recommended for dental procedures, as it causes serious, sometimes fatal reactions — 12,800 in the United States alone — including an increase in infections including Clostridium difficile, implant failure, bone regeneration failure and peri-implantitis.
Conclusion
Effective and judicious use of antibiotics makes them an important adjunct in the treatment of periodontal diseases, peri-implantitis and preventing implant failures.
Used appropriately, antibiotics can make a significant contribution to saving our patient’s teeth and implants.