Essential New Clinical, Diagnostic and Treatment Information
he first World Workshop on periodontics since 1999 was intended to account for the notable advancements in the diagnosis and treatment of periodontal disease in the past 18 years. In addition, the proceedings, for the first time, addressed the diagnosis and treatment of peri-implant diseases and conditions within the classifications of periodontal disease.
The World Workshop agreed a new classification system for periodontal and peri-implant diseases and conditions is necessary for clinicians to properly diagnose and treat patients, as well as for scientists to investigate etiology,pathogenesis, natural history, and treatment of the diseases and conditions.
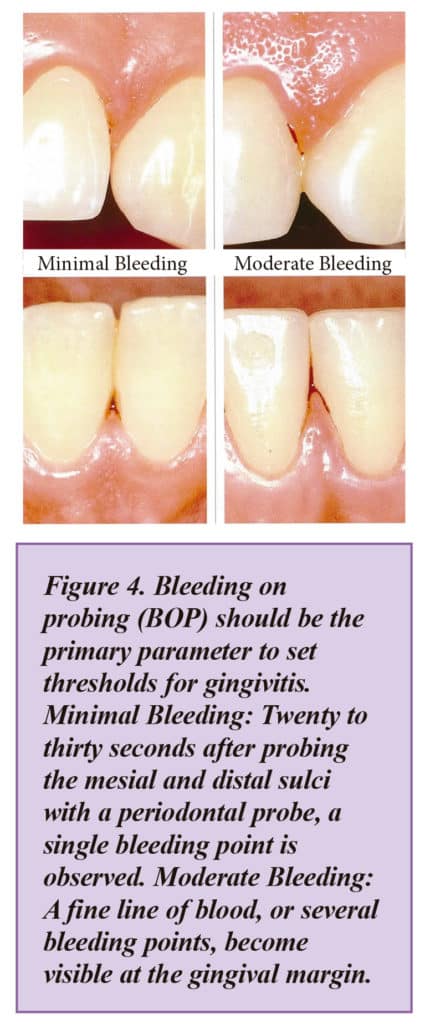
It agreed that bleeding on probing (BOP) should be the primary parameter to set thresholds for gingivitis. It agreed that a patient with gingivitis can revert to a state of health, but a periodontitis patient remains a periodontitis patient for life, even following successful therapy, and requires life-long supportive care to prevent recurrence of disease.
Studies investigated the predictive values of absence of BOP as an indicator for periodontal stability. While the positive predictive value remained rather low for repeated BOP prevalence less than 30 percent — the negative predictive value in the same studies was nearly 100 percent. The Workshop agreed this demonstrated that absence of BOP at repeated examinations represented periodontal health and was a very reliable indicator for periodontal stability.
A New Classification System for Periodontal Disease
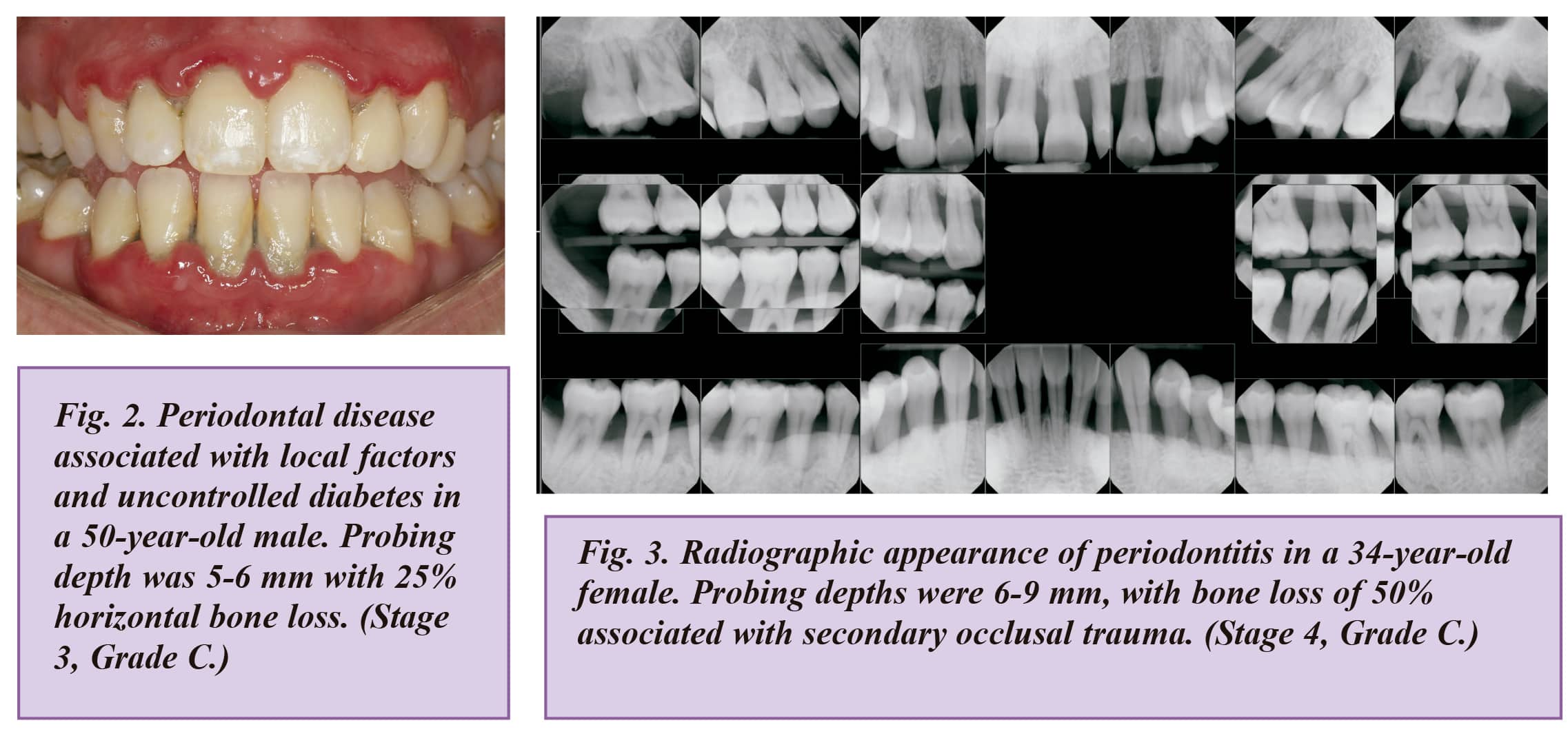
The Workshop agreed that, consistent with current knowledge on pathophysiology, three forms of periodontitis can be identified, and established the following new classification system for periodontal disease:
- Necrotizing periodontitis
- Periodontitis as a manifestation of systemic disease, and
- The forms of the disease previously recognized as “chronic” or “aggressive” periodontitis, now grouped under a single category, “periodontitis”.
In revising the classification system, the Workshop agreed on a classification framework for periodontitis, which would be further characterized by a multidimensional staging and grading system, and which could be adapted over time as new evidence emerges.
Staging was determined to be largely dependent upon the severity of disease at presentation, as well as on the complexity of disease management. Four stages, 1 through 4, are each to be determined after considering several variables, including clinical attachment loss, amount and percentage of bone loss, probing depth, presence and extent of angular bony defects, and furcation involvement, tooth mobility, and tooth loss due to periodontitis.
Grading was established to provide supplemental information about biological features of the disease, including a historybased analysis of the rate of disease progression, assessment of the risk for further progression, anticipated poor outcomes of treatment, and assessment of the risk that the disease or its treatment may negatively affect the general health of the patient.
Three grades were established:
- Grade A – low risk for progression
- Grade B – moderate risk for progression
- Grade C – high risk for progression
In addition to aspects related to the progression of periodontitis, grading factors are to include general health status, and other exposures, such as smoking or level of metabolic control in diabetes. Thus, grading will allow the clinician to incorporate individual patient factors into the diagnosis, which are crucial to comprehensive case management.
Summary of Additional Workshop Findings
Evidence Regarding the Favorable Influence of Periodontal Treatment on Systemic Diseases
Current evidence that effective treatment of periodontitis can favorably influence systemic diseases, although limited, is intriguing and should definitely be assessed. Several studies show that periodontitis contributes to the overall inflammatory burden, which is strongly implicated in heart disease, stroke and diabetes. Periodontal diseases can no longer be considered simple bacterial infections: rather, they are complex diseases of multifactorial nature involving an intricate interplay between the subgingival microbiota, host immune and inflammatory responses, and environmental modifying factors. Bacteria are necessary, but not sufficient, to cause disease in all people.
Occlusal Trauma and Periodontitis
Occlusal trauma does not initiate periodontitis, and there is weak evidence that it alters the progression of the disease. Reduction of tooth mobility may enhance the effect of periodontal therapy.
Occlusal Trauma and Gingival Recession
There is a lack of evidence from human studies implicating occlusal trauma in the cause or progression of gingival recession.
The Association of Removable or Fixed Appliances with Periodontitis
The available evidence does not support that optimal fixed or removable appliances are associated with periodontitis. However, evidence was found that prosthesis design can be associated with plaque retention, gingival recession and loss of periodontal support.
Occlusal Trauma and Abfractions
There is no credible evidence to support the theory that occlusal trauma causes abfractions. A possible cause of what dentists have been calling abfraction lesions is toothpaste abuse, according to Peter Dawson in Functional Occlusion 2007.
Keratinized Tissue and Periodontal Health
Periodontal health can be maintained in most patients under optimal oral conditions, even with minimal amounts of keratinized tissue. However, an increased risk for development or progression of gingival recession was found in cases presenting with thin periodontal phenotypes, suboptimal oral hygiene, and requiring restorative or orthodontic treatment.
Biologic Width Redefined
Biologic width was redefined as “supracrestal tissue attachment,” and this question was addressed: What is the ideal dimension, and does infringement cause loss of periodontal support?
- Histologically, the dimension is composed of junctional epithelium and supracrestal connective tissue attachment.
- The average dimensions for each varies histologically from 0.5 to 1 mm.
- Since it varies considerably, it is impossible to define a fixed biologic width dimension.
- Available evidence supports that infringement is associated with inflammation and loss of periodontal support.
New Classification for Mucogingival Defects Based on Interproximal Bone Levels
Mucogingival defects based on interproximal bone levels were placed into three new classifications.
- Recession Type 1 (RT1): Gingival recession with no loss of interproximal attachment. (This new classification combines Millers 1st and 2nd classifications.)
- Recession Type 2 (RT2): Gingival recession associated with loss of interproximal attachment. (This classification is the same as Millers 3rd classification.)
- Recession Type 3 (RT3): Gingival recession associated with a loss of interproximal attachment greater than the facial recession. (Miller’s 4th classification.)
(Miller has questioned combining his classifications I and II, saying this could be detrimental to the clinician attempting root coverage, since different procedures are required to treat Class I and Class II gingival recession.)
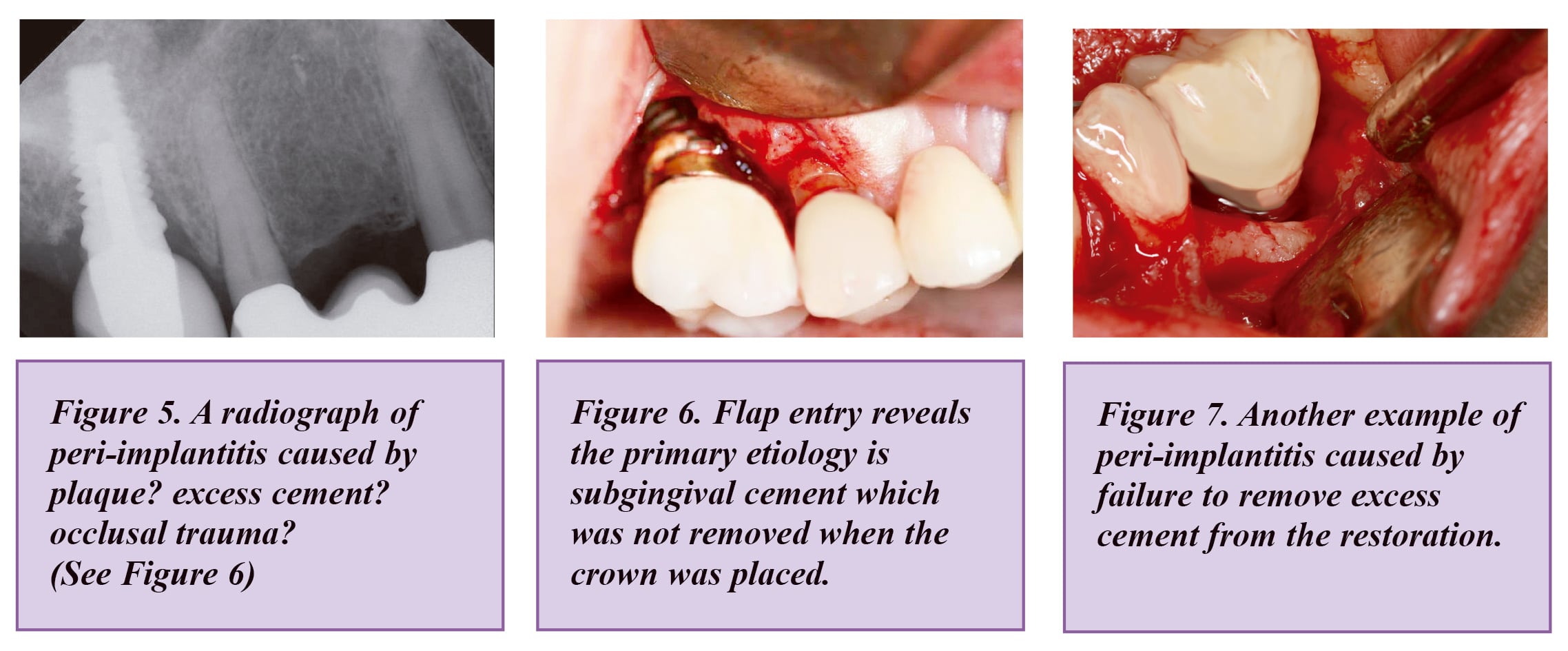
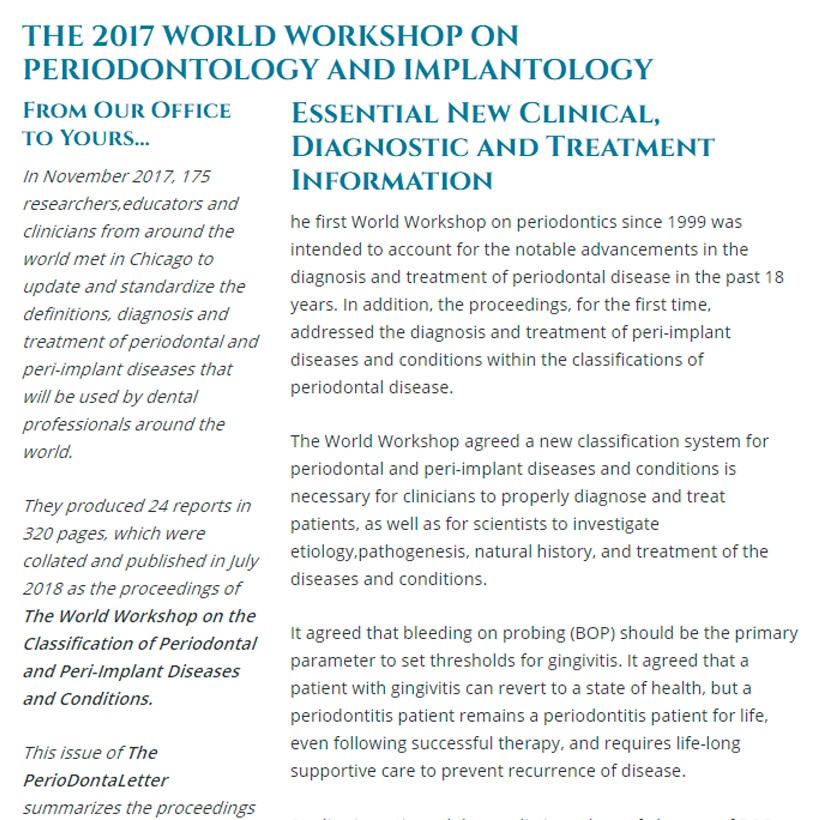
Peri-implantitis
The World Workshop defined periimplantitis as a plaque-associated pathologic condition occurring in the tissue around dental implants, characterized by inflammation in the peri-implant mucosa, and subsequent progressive loss of supporting bone. Peri-implant mucositis is assumed to precede peri-implantitis. Peri-implantitis was found to be associated with poor plaque control, and with patients with a history of severe periodontitis. The onset of periimplantitis may occur early, following implant placement, as indicated by radiographic data. Peri-implantitis, in the absence of treatment, seems to progress in a non-linear and circumferential, and accelerating pattern. Probing of peri-implant tissue with light force was determined to be a safe and important part of a complete oral examination.
A Common Finding in Infected Implants
When compared with healthy implant sites alone, peri-implantitis is associated with higher counts of 19 bacterial species, including Prophyromonas gingivalis and Tannerella forsythia. Several consensus statements concluded:
- Suppuration is a common finding at sites diagnosed with peri-implantitis.
- Anti-infective treatment strategies are successful in suppressing disease progression.
The Role of Titanium Particles Involved in Peri-Implantitis
Available evidence does not allow an evaluation of the role of titanium or metal particles in the pathogenesis of periimplant diseases.
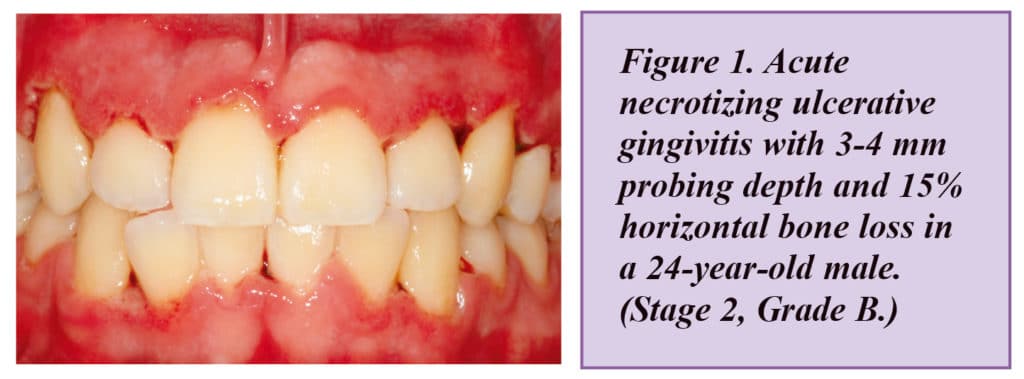
The Risk of Peri-Implantitis in Cement-Retained Restorations vs. Screw-Retained Implants
Properly cemented restorations with no excess cement were not found to be at higher risk for peri-implantitis when compared to screw-retained restorations. Certain cements are radiopaque and they should be used. Nevertheless, a systematic review emphasized the rough surface structure of cement remnants may facilitate retention of the bacteria which causes periimplantitis and biofilm formation.
Lack of Keratinized Gingiva as a Risk Factor for Peri-Implantitis
While studies suggest that the absence or a reduced width of keratinized gingiva may negatively affect self-performed oral hygiene measures, there is limited evidence that this factor constitutes a risk for peri-implantitis.
Periapical Lesions on Implants
The majority of studies reported a direct correlation between retrograde periimplantitis and the existence of periapical endodontic lesions at adjacent teeth. The scarce evidence available indicates that sites with periapical infections have survival and complication rates similar to implants placed in non-infected sites.
Occlusal Overload as a Risk Factor for Peri-Implantitis
There is currently no evidence that occlusal overload constitutes a risk factor/ indicator for the onset or progression of peri-implantitis. It did find that thin soft tissues lead to increased marginal bone loss compared to thick soft tissues at implants.
Discrepancies Between Implants And Teeth Over Time
Discrepancies between teeth and implants may develop due to tooth wear, and changes in the anatomy of the face and jaws, which occur continuously. In one study, the maxillary arch length decreased by an average of 5 mm, and the mandibular arch decreased by an average of 8 mm, between the ages of 13 and 45.
Peri-Implantitis Probing Depths
The results from available studies document that the peri-implant mucosa is about 3 to 4 mm high, and the epithelium is about 2 mm high. The zone of connective tissue averaged 1.5 mm. In the absence of previous radiographs, radiographic bone level loss of 3 mm or greater, and probing depths 6 mm or more. indicate peri-implantitis.
Conclusion: The Most Important Factors for Controlling Periodontitis and Peri-Implantitis
The Workshop concluded that adequate motivation in the patient’s own plaque control, and compliance with maintenance protocols, appear to be the most important factors in limiting or avoiding potential negative effects on the periodontium. It found there is evidence that poor plaque control and lack of regular maintenance constitute risk factors/ indicators for peri-implantitis.